What is acute renal failure?
It is the RAPID DECLINE in Glomerular Filtration Rate(GFR) over hours and days causing deterioration in renal function resulting to build-up of nitrogenous wastes. It causes a sudden retention of endogenous and exogenous substances (e.g. Nitrogenous wastes). Reduction in urine flow rate aka oliguria <400ml/day and electrolyte and acid-base abnormalities are its common symptoms/effects.
Classification
Acute renal failure is classified into three namely Prerenal, Intrarenal, and Postrenal renal failure. Prerenal ARF or azotemia causes renal hypoperfusion, resulting in decreased function without frank parenchymal damage which accounts for approximately ~55% of ARF cases. Intrinsic ARF directly involve the renal parenchyma ~40% of the cases. Postrenal ARF is associated with urinary tract obstruction~5% of the cases.
Prerenal Acute renal failure
It is the most common cause of community-acquired ARF due to history of poor fluid intake, treatment with Non-Steroidal Anti-inflammatory Drug (NSAID), ACE inhibitors/ARBs and worsening heart failure. Common features include blood volume depletion due to absolute/postural hypotension, low jugular venous pressure and dry mucus or it can be due to decreased effective circulatory volume(e.g., heart failure or liver disease) and decreased cardiac output.
— I. Hypovolemia
— A. Increased extracellular fluid losses: hemorrhage
— B. Gastrointestinal fluid loss: vomiting, diarrhea
— C. Renal fluid loss: diuretics, osmotic diuresis, hypoadrenalism
— D. Extravascular sequestration: burns, pancreatitis, severe hypoalbuminemia (hypoproteinemia)
— E. Decreased intake: dehydration, altered mental status
II. Altered renal hemodynamics resulting in hypoperfusion
— A. Low cardiac output state: diseases of the myocardium, valves, and pericardium (including tamponade); pulmonary hypertension or massive pulmonary embolism leading to right and left heart failure; impaired venous return (e.g., abdominal compartment syndrome or positive pressure ventilation)
— B. Systemic vasodilation: sepsis, antihypertensives, afterload reducers, anaphylaxis
— C. Renal vasoconstriction: hypercalcemia, catecholamines, calcineurin inhibitors, amphotericin B
— D. Impairment of renal autoregulatory responses: cyclooxygenase inhibitors (e.g., nonsteroidal anti-inflammatory drugs), angiotensin-converting enzyme inhibitors, or angiotensin II receptor blockers
— E. Hepatorenal syndrome
Causes of Intrarenal acute renal failure
II. Parenchymal (Intrarenal)
1. Specific
a. Glomerulonephritis
b. Interstitial nephritis
c. Toxin, dye-induced
2.Nonspecific
a. Acute tubular necrosis
b. Acute cortical necrosis
I would like to give particular attention on acute tubular necrosis .It is the death of the tubules inside of our kidney and this could be detrimental to the overall function of our kidney. What causes acute tubular necrosis?
— A. Ischemia: causes are the same as for prerenal ARF, but generally the insult is more severe and/or more prolonged
— B. Infection, with or without sepsis
— C. Toxins:
— 1. Exogenous: radiocontrast, calcineurin inhibitors, antibiotics (e.g., aminoglycosides), chemotherapy (e.g., cisplatin), antifungals (e.g., amphotericin B), ethylene glycol
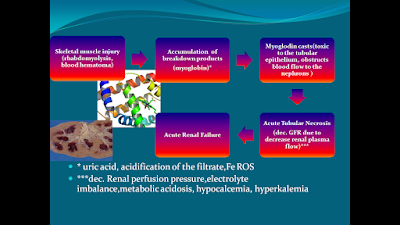
This illustration tells you how severe beating/ hazing or any intense muscular injury could lead to acute renal failure which could be fatal.
Causes of Postrenal Acute Renal Failure
III. Postrenal -obstruction to the flow of urine
1. Calculus in patients with solitary kidney
2. Bilateral ureteral obstruction
3. outlet obstruction
4. Leak, posttraumatic
MANAGEMENT
Prerenal ARF
>Hypotonic solutions (e.g., 0.45% saline) are usually recommended as initial replacement in patients with prerenal ARF due to increased urinary or gastrointestinal fluid losses(Fluid replacement).
>isotonic saline may be more appropriate in severe cases
> Cardiac failure may require aggressive management with ionotropic agents, preload and afterload reducing agents, antiarrhythmic drugs, and mechanical aids such as intraaortic balloon pumps
INTRINSIC ARF
>Many different approaches to attenuate injury or hasten recovery for ischemic and nephrotoxic AKI failed.....
>Acute glomerulonephritis or vasculitis may respond to immunosuppressive agents (glucocorticoids, alkylating agents, and/or plasmapheresis, depending on the primary pathology).
POSTRENAL ARF
> requires close collaboration between nephrologist, urologist, and radiologist.
>Obstruction of the urethra or bladder neck is usually managed initially by transurethral or suprapubic placement of a bladder catheter, which provides temporary relief while the obstructing lesion is identified and treated definitively.
>Similarly, ureteric obstruction may be treated initially by percutaneous catheterization of the dilated renal pelvis or ureter.
>Obstructing lesions can often be removed percutaneously (e.g., calculus, sloughed papilla) or bypassed by insertion of a ureteric stent (e.g., carcinoma).
>Most patients experience an appropriate diuresis for several days following relief of obstruction.
No comments:
Post a Comment